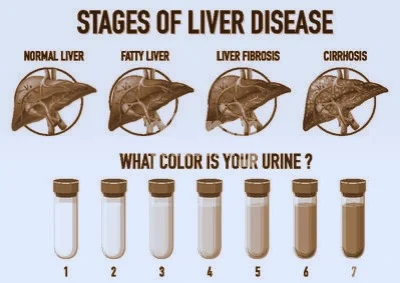
The Stages of Liver Disease
The liver, a vital organ, plays an essential role in various bodily functions, including detoxification, protein synthesis, and the production of biochemicals necessary for digestion. Despite its resilience and ability to regenerate, the liver can suffer damage that, if left untreated, can progress through several stages, each more severe than the last. Understanding these stages is crucial for early intervention and effective treatment.
Stage 1: Steatosis (Fatty Liver)
The initial stage of liver disease is steatosis, commonly known as fatty liver. This condition occurs when fat accumulates in the liver cells, leading to inflammation and liver enlargement. Steatosis can result from various factors, including excessive alcohol consumption, obesity, diabetes, and high cholesterol. It is often asymptomatic, making early detection challenging.
However, some individuals may experience fatigue, weakness, and discomfort in the upper right abdomen. Lifestyle changes, such as a healthy diet, regular exercise, and avoiding alcohol, can reverse fatty liver. If left unchecked, it can progress to more severe stages of liver disease.
Stage 2: Steatohepatitis
When fatty liver progresses, it can lead to steatohepatitis, characterized by inflammation and damage to liver cells. This stage includes two types: alcoholic steatohepatitis (ASH), caused by excessive alcohol consumption, and nonalcoholic steatohepatitis (NASH), which is unrelated to alcohol use and often associated with obesity, insulin resistance, and metabolic syndrome.
Symptoms of steatohepatitis may include fatigue, abdominal pain, and jaundice (yellowing of the skin and eyes). Blood tests may show elevated liver enzymes, indicating liver inflammation. A liver biopsy is often required to confirm the diagnosis.
Treatment focuses on addressing the underlying causes. For ASH, quitting alcohol is crucial. For NASH, weight loss, managing diabetes, and controlling cholesterol levels are essential steps. Medications and lifestyle changes can help manage inflammation and prevent further liver damage.
Stage 3: Fibrosis
Fibrosis occurs when persistent inflammation and liver damage lead to the formation of scar tissue. Unlike healthy liver tissue, scar tissue cannot perform vital liver functions, leading to decreased liver efficiency. Fibrosis can develop silently over years, with few or no symptoms.
As the scar tissue accumulates, the liver becomes stiffer, and blood flow through the liver is restricted. This can cause portal hypertension, where increased blood pressure in the portal vein leads to complications like varices (enlarged veins) in the esophagus and stomach.
A liver biopsy is the gold standard for diagnosing fibrosis, but non-invasive methods like elastography (FibroScan) and blood tests (FibroTest) are increasingly used. Early fibrosis can be managed with lifestyle changes, medications to reduce liver inflammation, and treating the underlying causes. However, advanced fibrosis requires more intensive treatment and monitoring.
Stage 4: Cirrhosis
Cirrhosis represents severe liver damage where extensive scarring has replaced much of the healthy liver tissue. This stage significantly impairs liver function and can lead to life-threatening complications. Cirrhosis can result from chronic alcohol abuse, viral hepatitis (hepatitis B and C), NASH, and other chronic liver diseases.
Symptoms of cirrhosis can be mild initially but progress as liver function declines. Common symptoms include fatigue, weakness, loss of appetite, weight loss, nausea, swelling in the legs and abdomen (ascites), and jaundice. Advanced cirrhosis can cause complications like hepatic encephalopathy (confusion and cognitive impairment due to liver dysfunction), variceal bleeding, and liver cancer.
Diagnosing cirrhosis involves imaging tests (ultrasound, CT scan, MRI), blood tests, and liver biopsy. Treatment focuses on managing symptoms, preventing complications, and slowing disease progression. Lifestyle changes, such as avoiding alcohol and maintaining a healthy weight, are crucial. Medications may be prescribed to manage symptoms and complications. In severe cases, a liver transplant may be the only option.
Stage 5: End-Stage Liver Disease (ESLD)
End-stage liver disease (ESLD) is the final stage of chronic liver disease, where the liver can no longer perform its essential functions. At this point, the liver has extensive scar tissue, and complications are severe and life-threatening. Common causes of ESLD include advanced cirrhosis, chronic viral hepatitis, and genetic liver diseases.
Symptoms of ESLD are severe and can include profound fatigue, confusion (hepatic encephalopathy), severe jaundice, significant fluid accumulation in the abdomen (ascites), and frequent infections. Patients with ESLD are at high risk for liver cancer and other serious complications.
Management of ESLD involves supportive care to manage symptoms and complications. This includes medications to reduce fluid buildup, manage infections, and treat hepatic encephalopathy. Nutritional support and managing electrolyte imbalances are also essential.
Liver transplantation is often the only definitive treatment for ESLD. Candidates for transplantation undergo thorough evaluation to determine their suitability for the procedure. Post-transplant, patients require lifelong immunosuppressive therapy to prevent organ rejection.
Preventing and Managing Liver Disease
Preventing liver disease involves lifestyle choices that promote liver health. These include:
1. **Avoiding excessive alcohol consumption:
Limiting alcohol intake reduces the risk of ASH and other alcohol-related liver diseases.
2. **Maintaining a healthy weight:
Obesity is a significant risk factor for fatty liver disease and NASH.
3. **Healthy diet:
A balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports liver health.
4. **Regular exercise:
Physical activity helps maintain a healthy weight and reduces the risk of metabolic syndrome.
5. **Avoiding risky behaviors:
Reducing exposure to hepatitis B and C through safe practices, such as not sharing needles and practicing safe sex, prevents viral hepatitis.
6. **Vaccinations:
Hepatitis A and B vaccines can prevent these viral infections.
7. **Regular medical check-ups:
Monitoring liver health through regular blood tests and check-ups can detect liver disease early.
Conclusion
Liver disease progresses through distinct stages, each more severe than the last. Early detection and intervention are crucial for preventing the progression of liver disease and managing its complications. By understanding the stages of liver disease and adopting healthy lifestyle choices, individuals can protect their liver health and improve their overall well-being. If you suspect you have liver disease, it is essential to seek medical advice promptly to receive appropriate care and treatment.
Want More Great Quotes? Check Out…
👇👇
#The Health Benefits of Vitamin D Foods: A Comprehensive Overview
#High Cholesterol: Symptoms, Risks, and Management
#Nutrition Essentials: Fueling Your Body for Strong Bones"
#A Comprehensive Guide to TikTok Ads"
# Why is healthcare an issue in America?
#"Life Expectancy and Quality of Life: Navigating a Positive Future with HIV"
#"Investigating the Gap: Understanding Substance Abuse and Creating Approaches to Recovery"
#How To Fit In 40 Age."Unlocking the Fountain of Youth: A Guide to Fitness at 40 and Beyond"
#How To Cover Out Over Weight And Obesity
20 Simple Mind Activities to Work on Your Memory
Why I Exercise: Real People Weigh In on What Keeps Them going
Prosperity Experts Figure out How Yo Consuming less calories Affects Your Body
.png)
.png)











0 Comments